Spine Surgeon
Spine Infection Treatment Mumbai
Spine infections
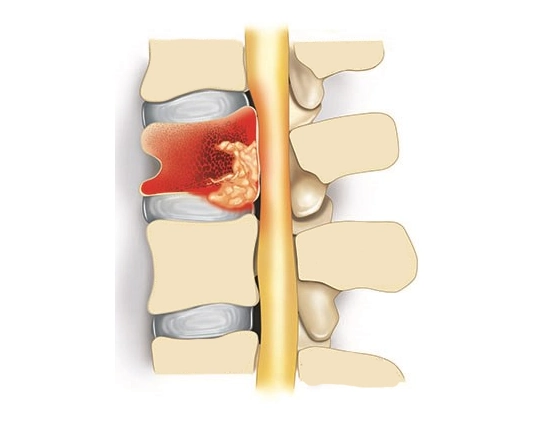
Spine infections are serious medical conditions that involve the invasion of bacteria, viruses, or fungi into the spinal structures.
These infections can affect various parts of the spine, including the vertebrae, intervertebral discs, spinal cord, and surrounding soft tissues. Spine infections can lead to significant pain, neurological deficits, and potentially life-threatening complications if left untreated.
Prompt diagnosis and appropriate treatment are essential to prevent further damage and improve outcomes for individuals affected by spine infections.
What are the types of spine infections?
Bacterial spinal infections: These infections are predominantly caused by bacteria, particularly Staphylococcus aureus, which infiltrate the bones, soft tissues, and discs of the spine. They can manifest as either acute or chronic conditions and may lead to complications such as vertebral osteomyelitis, epidural abscess, or discitis.
Tuberculous spinal infections: Mycobacterium tuberculosis is responsible for this type of infection, commonly known as Pott’s disease. It affects the vertebrae and spinal discs, potentially resulting in vertebral collapse and spinal deformities.
Viral spinal infections: These infections stem from viruses such as the herpes simplex virus, which target the spinal nerves and give rise to conditions like shingles or viral meningitis.
Fungal spinal infections: Infections caused by fungi like Aspergillus or Candida primarily affect the spine and nearby tissues. Although rare, they pose significant challenges in treatment, often requiring long-term medication.
Postoperative infections: These infections occur subsequent to spinal surgery, typically when bacteria enter the surgical site during or after the procedure.
Spinal abscess: These infections involve the accumulation of pus within the spinal column or its surrounding tissues, resulting from bacterial, fungal, or other microbial sources.
What are the causes and symptoms of spine infections?
Causes of Spinal Infections
- Weakened Immune System: Conditions or situations that compromise the body’s immune response, such as immunodeficiency disorders, chronic illnesses, or certain medications, can increase susceptibility to spinal infections.
- Bloodstream Infections: Bacteria or fungi entering the bloodstream from other parts of the body, such as urinary tract infections, respiratory infections, or skin infections, can travel to the spine and cause infection.
- Trauma or Injury: Penetrating injuries or fractures to the spine can create openings for pathogens to enter, leading to infection.
- Underlying Medical Conditions: Conditions such as diabetes, HIV/AIDS, or cancer can weaken the immune system and predispose individuals to spinal infections.
- Intravenous Drug Use: Sharing contaminated needles or injection equipment increases the risk of bloodstream infections, which can lead to spinal infections.
- Invasive Medical Procedures: Certain medical interventions, such as spinal injections or catheterizations, can introduce microorganisms into the spinal area, potentially causing infection.
- Age: Older adults and infants are more susceptible to infections due to age-related changes in immune function.
Symptoms of spine infection
- Localized Pain: Persistent, severe pain in the affected area of the spine.
Fever and Chills: Systemic symptoms indicating an ongoing infection. - Neurological Symptoms: Weakness, numbness, or tingling in the arms, legs, or trunk due to nerve compression.
- Limited Mobility: Difficulty moving the spine or experiencing stiffness.
- Swelling and Tenderness: Inflammation and tenderness around the affected area of the spine.
Restricted Range of Motion: Difficulty bending or twisting the spine due to pain and stiffness. - Fatigue: Generalized weakness or malaise often accompanying infections.
- Muscle Spasms: Involuntary contractions of muscles around the spine, contributing to pain and discomfort.
- Visible Deformities: In severe cases, spinal deformities such as kyphosis or scoliosis may be noticeable.
- Bladder or Bowel Dysfunction: In advanced cases, spinal infections can lead to urinary or fecal incontinence due to nerve compression.
How to diagnose spine infection?
- X-rays: These may reveal changes in the bone density or alignment, but they are not very sensitive for detecting early-stage infections.
- MRI (Magnetic Resonance Imaging): Provides detailed images of the spine, including soft tissues like the spinal cord, nerves, and discs. MRI is highly sensitive for detecting spinal infections.
- CT (Computed Tomography) scan: Can provide detailed images of the bones and soft tissues, helpful for evaluating bony abnormalities and abscesses.
- Blood tests: Elevated white blood cell count and inflammatory markers (e.g., erythrocyte sedimentation rate, C-reactive protein) may indicate an infection.
- Cultures: Samples of blood, urine, or spinal fluid may be collected and sent for laboratory analysis to identify the causative organism.
- Biopsy: If imaging and laboratory tests are inconclusive, or if a specific diagnosis is needed, a biopsy of the affected area may be performed. A small sample of tissue is removed and examined under a microscope to identify the organism causing the infection.
- Other Tests: Depending on the suspected cause of the infection and the individual’s medical condition, additional tests such as a lumbar puncture (spinal tap) may be performed to evaluate spinal fluid for signs of infection.
What are the treatment options for spine infections?
Antibiotic Therapy:
Administer IV antibiotics initially, followed by oral antibiotics for long-term treatment, tailored based on bacterial sensitivity.
Surgical Intervention:
Drain abscesses surgically, perform debridement to remove infected tissue, decompress spinal cord and nerves, and stabilize the spine with fusion surgery if necessary.
Pain Management:
Utilize medications like NSAIDs and opioids, consider physical therapy, and provide supportive devices such as braces for pain relief.
Monitoring and Follow-Up:
Schedule regular appointments to monitor treatment response, watch for complications, and adjust the treatment plan accordingly.
For Spine Infection Treatment Mumbai or spinal tuberculosis, contact Spine Synapse, Mumbai’s premier spine hospital. Schedule an appointment today with our top spine doctors.