Can physiotherapy alone get you back on your feet—or will an L4–L5 disc bulge eventually need surgery? In India, low back pain is a leading cause of lost workdays, and many cases involve the L4–L5 level. For a large number of patients, a structured, therapist-guided program can calm nerve irritation, restore mobility, and keep you out of the operating room. The keys are timing (start early), personalization (treat your pattern, not a generic routine), and consistency (progress week by week).
When conservative care isn’t enough, Synapse Spine—a top center with some of the best spine surgeons in India—provides minimally invasive options (endoscopic and microscope-assisted) alongside integrated rehabilitation, so your non-surgical spine treatment and surgical pathway stay coordinated from day one.
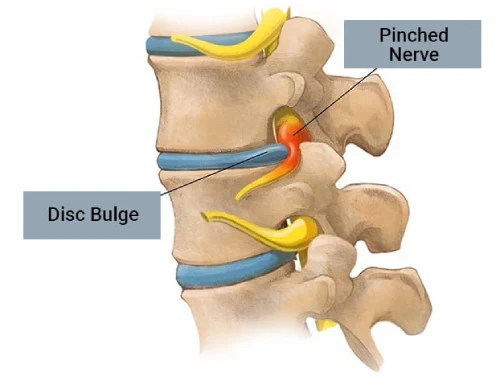
What Is an L4–L5 Disc Bulge?
Between each pair of vertebrae is a disc that acts like a shock absorber. At L4–L5, the disc is subjected to heavy daily loads (sitting, bending, lifting). With time or sudden strain, the disc may bulge or herniate, narrowing the space for the existing nerves. This can trigger lumbar radiculopathy—shooting leg pain (sciatica), tingling, numbness, and sometimes weakness. Not every bulge needs surgery: many settle with the right non-surgical spine treatment plan.
Can Physiotherapy “Cure” an L4–L5 Disc Bulge?
“Cure” depends on what you mean:
- Pain & function: For the majority with mild–moderate nerve irritation (no progressive weakness, no red flags), physiotherapy for disc bulge can reduce inflammation, improve mechanics, and return you to normal life without surgery.
- Disc anatomy: A bulge may not “vanish” on MRI quickly. But your symptoms can resolve as swelling reduces, muscles balance, and movement patterns improve. Some herniations do shrink over months.
- Durability: With consistent exercises and ergonomic changes, many patients remain well long-term.
In practice, physiotherapy often “cures the problem you feel”—pain and disability—even if the picture on MRI takes longer to change.
How Physiotherapy Works for L4–L5: The Four Pillars
- Pain modulation & nerve calming
– Gentle neural mobilization (“nerve glides”)
– Anti-inflammatory strategies (positions of relief, taping) - Segmental stability
– Deep core activation (transversus abdominis, multifidus)
– Hip and glute strengthening to unload the lumbar segment - Mobility without irritation
– Hip flexor and hamstring flexibility to prevent compensatory lumbar stress
– Thoracic mobility to reduce hingeing at L4–L5 - Motor control & habit change
– Posture re-training (sitting, standing, lifting, driving)
– Graded return to walking, stairs, and sport
When these pillars are individualized and progressed, nerve pressure decreases, muscles share load better, and pain settles—often within weeks.
What a Good Physio Plan Looks Like (Weeks 0–12)
Weeks 0–2 : pain-relieving positions (slight lumbar extension or flexion bias, as tested), unloading postures, short walks, basic core “breathing + bracing,” gentle nerve glides, ice/heat as advised.
Weeks 3–6 : progressive core (dead bug, bird-dog, side planks), hip/glute strength (bridges, clams, step-ups), mobility blocks (hip flexor/hamstring work), posture drills for desk and car.
Weeks 7–12 : loaded patterns (hip hinge, squat variants), endurance walking/cycling, return-to-run/sport progressions if relevant, relapse-prevention checklist.
Tip: Expect 2–3 supervised sessions/week early, then taper to home-led programs. Consistency beats intensity.
When Physiotherapy Is Enough—And When It’s Not?
Physio typically succeeds when:
- Pain is mechanical (varies with position), leg strength is stable, and there’s no saddle numbness or bladder/bowel change.
- Symptoms improve 10–30% within 2–3 weeks of a guided plan.
- You can progressively increase activity with fewer flare-ups.
Consider escalation when:
- Pain remains severe and unresponsive after 6–8 weeks of evidence-based rehab.
- There’s progressive weakness (e.g., foot drop), or intolerable neural pain blocking sleep and rehab.
Escalation doesn’t always mean surgery. Image-guided injections can be a bridge that allows therapy to proceed. Surgery is reserved for clearly indicated cases.
Red Flags: Don’t Delay Medical Attention
- New urinary retention/incontinence or bowel changes
- Saddle anesthesia (numbness in the groin/perineal area)
- Rapidly worsening leg weakness, falls, or foot drop
- Fever, unexplained weight loss, trauma, cancer history
If any of these occur, get urgent evaluation before continuing therapy.
Home & Lifestyle: Small Habits, Big Results
- Desk setup: screen at eye level; hips/knees ≈ 90°; lumbar support; feet flat
- Movement snacks: stand or walk 2–3 minutes every 30–45 minutes
- Walk daily: begin with 10–15 minutes; add 5 minutes every 3–4 days as tolerated
- Smart lifting: hinge at hips, keep load close, avoid twist-and-lift combos
- Sleep positions: side-lying with pillow between knees or supine with knees slightly elevated
- Anti-inflammatory basics: prioritize protein, hydration, and regular sleep; stop smoking
Myths vs Facts
- Myth: “A bulging disc always needs surgery.”
Fact: Most improve with non-surgical spine treatment and time. - Myth: “Rest until pain disappears.”
Fact: Gentle, graded movement helps nerves calm and prevents deconditioning. - Myth: “Core = endless crunches.”
Fact: Lumbar-friendly core (bracing, dead bug, bird-dog, side plank) is safer and more effective.
Exercise (To Be Individualized)
- Relief positions: prone on elbows or knees-to-chest (whichever eases symptoms)
- Core activation: abdominal bracing with diaphragmatic breathing → dead bug → bird-dog
- Glute/hip strength: bridges (progress to single-leg), clamshells, lateral walks, step-ups
- Mobility: hip flexor stretch, hamstring sliders, thoracic rotations
- Nerve glides: sciatic sliders (low-amplitude, therapist-guided to avoid flare)
- Cardio: walking/cycling intervals without symptom provocation
Always get a licensed physiotherapist to tailor load, range, and frequency to your presentation.
Expected Timeline & Outcomes
- 2–3 weeks: pain modulation, fewer sharp flares, better sitting tolerance
- 4–6 weeks: strength and endurance rising; return to light recreational activity
- 8–12 weeks: confident lifting mechanics; near-normal routine for many patients
- Beyond 12 weeks: consolidation; MRI changes (if any) may lag behind symptom relief
Every case is unique: age, job demands, diabetes, smoking, and stress influence pace and prognosis.
Success Stories of Patient at Synapse Spine
- Desk Professional, 36: severe sciatica during deadlines; 8-week core/hip program + desk ergonomics → pain-free, back to gym with deadlifts under coaching.
- New Mom, 32: recurrent flares from bending/lifting; hip hinge retraining + glute strength + stroller-walk intervals → zero flares in 3 months.
- Logistics Worker, 48: couldn’t tolerate long drives; nerve glides + pacing + hamstring work → back to interstate routes with planned breaks.
Synapse Spine – Why Choose Us?
Best Spine Clinic in Mumbai, accessible to all, transcending the barriers of location and affordability. Our commitment extends beyond our clinic walls, reaching out through partnerships with trusted hospitals, NGOs, peripheral clinics, and outreach programs to ensure everyone receives the care they deserve.
Our team is composed of highly qualified doctors, each a testament to excellence, having honed their skills in premier institutes in India and abroad. Our doctors are not just practitioners but pioneers, actively engaged in cutting-edge research, dedicated charity work, and academic teaching. This rich blend of clinical practice and continual learning ensures that our patients receive care that is both compassionate and based on the latest advances in spine health.
We provide advanced minimally invasive spine care using:
- Endoscopic Spine Surgery
- Operating Microscope
- Neuromonitoring
- Ultrasonic Bone Scalpel
At Synapse Spine Best Spine Clinic in Mumbai, we blend the expertise of Orthopedic Spine and Neurospine Surgeons to address all spine ailments comprehensively. Our guiding principle is that most spine conditions can be effectively managed without surgery. We prioritize non-surgical treatments, viewing surgery as a last resort, only when absolutely necessary.
We value the spine’s critical role in every individual’s life and dedicate ourselves to personalized, non-invasive therapies. Our philosophy is about compassionate, innovative care, aiming to improve lives by prioritizing patient well-being and minimally invasive solutions for spine health.
FAQs About Physiotherapy & L4–L5 Disc Bulge (7)
How soon should I start physio after an acute flare?
Within a few days, once severe pain is controlled—early guided movement helps.
Can I do exercises from YouTube?
Use them only after a therapist confirms they match your pattern; wrong drills can flare symptoms.
Will a brace help?
Short-term use may help some, but long-term reliance can weaken support muscles.
Is walking safe?
Usually yes—start short and frequent; progress by time, not speed.
Do I need an MRI first?
Not always. If there are no red flags and signs fit a disc pattern, a trial of care is reasonable. MRI is useful when symptoms persist or escalate.
When is surgery the better choice?
Progressive weakness, intractable nerve pain despite optimal therapy, or any red flag affecting bladder/bowel or saddle sensation.
Will my disc “go back in place”?
Symptoms often resolve before imaging normalizes. Function, not the picture, is the primary goal.
Book Your Consultation Today
Symptoms often resolve before imaging normalizes. Function, not the picture, is the primary goal.
Our Synapse Spine Clinic is located in Vasai, Bandra, Andheri, Mira Road, Vile Parle, Chembur, Borivali, and Virar.
📞 Contact Numbers with call button for each number:
+91 81698 45056 | +91 93726 71858 | +91 93211 24611 | +91 74998 98303

