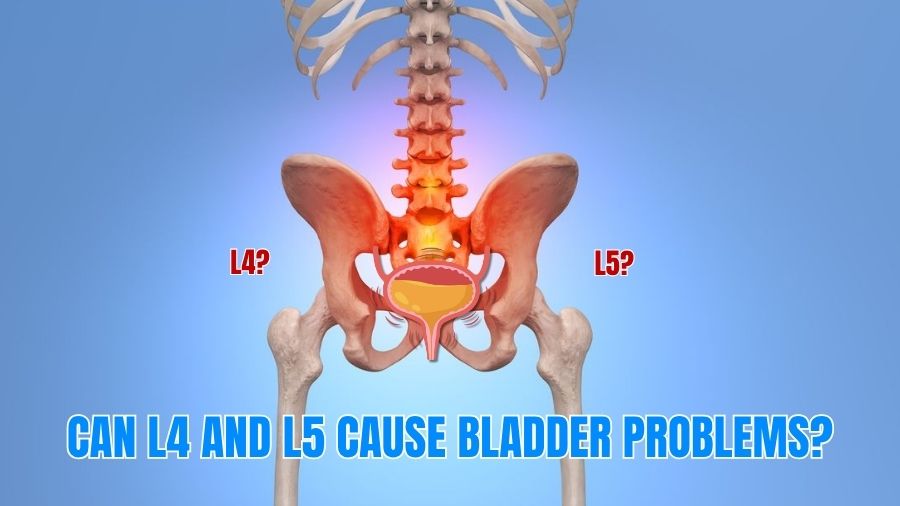
Did you know that over 20% of Indians above 40 suffer from lumbar spine disorders, and nearly 10–15% of those with severe L4–L5 disc herniation also report urinary symptoms ? Lumbar Disc Herniation – StatPearls – NCBI Bookshelf
Many people treat bladder problems separately without realizing they could be linked to the spine. So, the big question is: Can L4 and L5 cause bladder problems? The answer is yes—because the L4–L5 region is closely linked to spinal nerve compression and can even lead to conditions like cauda equina syndrome.At Synapse Spine – Best Spine Clinic in Mumbai, we believe in accessible, advanced, and compassionate care. With world-class expertise, minimally invasive solutions, and a philosophy that values non-surgical treatment first, Synapse Spine is redefining how spine care is delivered in India.
Why the L4–L5 Level Matters?
Your lumbar spine (L1–L5) bears most of your body’s load and enables bending, lifting, and twisting. The L4–L5 disc is one of the most stressed segments and, therefore, one of the most likely to bulge or herniate. When disc material presses on the nerve roots in the canal, it can cause spinal nerve compression—producing back pain, sciatica, numbness, and in select cases bladder dysfunction if the compression extends to the cauda equina or impacts sacral pathways that coordinate bladder contraction and sphincter control.
The Spine–Bladder Connection: What’s Actually Happening?
The bladder is governed by an elegant network of nerves. Lumbar and sacral roots (especially S2–S4) carry signals that allow you to sense bladder fullness and start/stop urination. When L4–L5 disc herniation narrows the canal or compresses the nerve bundle called the cauda equina, these signals are disrupted. Patients can feel frequency/urgency, a weak stream, difficulty initiating urination, incomplete emptying—or, in severe cases, painless retention with overflow leakage. Clinical reviews and urodynamic studies confirm this link: a sizable proportion of people with lumbar disc disease show measurable bladder dysfunction on testing.
Typical Symptoms When L4–L5 Affects Bladder Function
Watch for combinations of:
- Low back pain with sciatica (shooting pain down one or both legs)
- Numbness/tingling in buttocks, inner thighs, or perineal (“saddle”) region
- New urinary urgency, hesitancy, weak stream, or leakage
- A sense of incomplete emptying—or inability to pass urine at all
- New bowel dysfunction or sexual dysfunction
These symptoms range from subtle to dramatic. When they come on suddenly, or you develop urinary retention with saddle numbness, think of cauda equina syndrome and seek emergency care. Bladder dysfunction is reported in a high proportion of cauda equina presentations, and time to decompression strongly influences recovery.
Red Flags You Must Not Ignore
Call emergency services or go to a hospital now if you experience:
- Acute urinary retention or new loss of bladder/bowel control
- Saddle anesthesia (numbness in the area that would sit on a saddle)
- Rapidly worsening leg weakness or foot drop
Clinical guidance emphasizes that delayed treatment can lead to irreversible urinary retention and chronic incontinence; early recognition improves outcomes.
How Doctors Confirm the Spine–Bladder Link?
A careful work-up will typically include:
- MRI of the lumbar spine: shows L4–L5 disc herniation and degree of canal/nerve root compromise
- Focused neurological exam: maps sensory loss, reflex changes, and motor weakness
- Urodynamic studies: measure bladder storage and emptying patterns; abnormal results are common in disc disease with neurogenic bladder features.
- EMG (when needed): evaluates the electrical activity of pelvic floor and lower-limb muscles to support the diagnosis
Treatment Spectrum: From Conservative Care to Precision Surgery
1) Conservative options (for mild to moderate compression):
Targeted medications, guided physiotherapy, posture/ergonomics, and bladder training may stabilize symptoms and improve function when neurological compromise is limited.
2) Minimally invasive decompression (for significant compression or red flags):
Procedures like microdiscectomy or endoscopic decompression remove the offending disc fragment and free the nerves. In cauda equina syndrome, urgent surgical decompression is the standard of care; studies document high rates of bladder involvement at presentation and variable long-term recovery that correlates with timely surgery.
3) Rehabilitation and pelvic floor therapy:
After nerve decompression, pelvic floor physiotherapy and timed voiding can accelerate return of bladder control, while core strengthening protects the operative level.
What If You Wait? Potential Complications
Delaying care when bladder symptoms are present can cause:
- Persistent or permanent neurogenic bladder
- Chronic urinary tract infections (from retention/incomplete emptying)
- Progressive leg weakness and gait instability
- Chronic neuropathic pain
In short: if you have back/leg symptoms plus bladder changes, don’t “watch and wait.” Get evaluated promptly.
What do our Patients say?
“My L4–L5 disc herniation caused bladder urgency—after endoscopic decompression at Synapse Spine, control returned within weeks.”
— Ramesh K.
“Sciatica with hesitancy from L4–L5 compression—physio plus a microdiscectomy ended the bladder issues and leg pain.”
— Priya S.
“Months of retention due to L4–L5 nerve pressure—minimally invasive surgery and rehab restored my independence.”
— Abdul H.
Synapse Spine – Best Spine Clinic in Mumbai
Best Spine Clinic in Mumbai, accessible to all, transcending the barriers of location and affordability. At Synapse Spine, the commitment extends beyond clinic walls through partnerships with trusted hospitals, NGOs, peripheral clinics, and outreach programs—so people from diverse neighborhoods and budgets can access advanced care.
What we use to protect nerves and speed recovery:
- Endoscopic Spine Surgery (keyhole access, faster mobilization)
- Operating Microscope (magnified precision)
- Neuromonitoring (real-time nerve safety)
- Ultrasonic Bone Scalpel (selective bone cutting with minimal collateral tissue impact)
Most spine conditions can be managed without surgery; surgery is reserved only when absolutely necessary. Care plans emphasize personalized, non-invasive therapies, clear goals, and long-term spine health.
Who Is Most at Risk—and Why It’s So Common in India?
Sedentary work, prolonged sitting, improper lifting, and smoking all accelerate disc wear. Community studies in India point to substantial lifetime exposure to back pain across rural and urban populations; low back pain is consistently ranked among the top causes of years lived with disability.
Younger adults are increasingly affected too, likely due to long screen time, deconditioning, and nutrition factors, with clinicians noting a rise in symptomatic “slipped discs” among 20–35-year-olds.
Practical Prevention: Protect Your L4–L5 Segment
- Posture: neutral spine while sitting; hips and knees at 90°, screen at eye level
- Movement breaks: stand or walk 2–3 minutes every 30–45 minutes
- Core strength: supervised exercises to support the lumbar segments
- Smart lifting: hinge at hips, keep load close, avoid twisting under load
- Lifestyle: stop smoking; maintain vitamin D and overall nutrition for bone/disc health
These steps won’t cure a large herniation, but they meaningfully reduce risk and support recovery after treatment.
Frequently Asked Questions
Does every L4–L5 disc bulge cause bladder problems?
No. Many bulges are asymptomatic or cause only back/leg pain. Bladder issues tend to appear when there is significant nerve compression or evolving cauda equina syndrome.
What bladder symptoms are most concerning?
New urinary retention (can’t pass urine), incontinence, or saddle numbness are red flags—seek emergency care to rule out cauda equina.
How common is bladder dysfunction with disc disease?
Urodynamic abnormalities have been reported in a substantial fraction of patients with lumbar disc disease, and bladder dysfunction is frequent in cauda equina syndrome presentations.
Can bladder function recover after surgery?
Yes—especially when decompression is timely. Delays reduce the chance of full recovery.
Do I need a urologist or a spine specialist?
Both may be involved. If bladder changes accompany back/leg symptoms, start with a spine specialist for imaging and neurological assessment; urology testing can complement the plan.
Are modern surgeries truly “minimally invasive”?
Yes. Microdiscectomy and endoscopic approaches use small incisions, limit muscle disruption, and typically shorten hospital stay and rehab time when properly indicated.
If my symptoms are mild, can I try physiotherapy first?
Often, yes. For non-progressive symptoms without red flags, a trial of conservative care is standard. But if bladder symptoms escalate or new weakness appears, escalate care quickly.
Why Choose Synapse Spine for L4–L5 Problems?
At Synapse Spine, orthopedic spine and neurospine surgeons work together so that complex L4–L5 cases—especially those with bladder involvement—are managed comprehensively. What patients value most:
- Non-surgery-first mindset with clear thresholds for intervention
- Access to precision tools (endoscopic systems, microscope, neuromonitoring)
- Integrated physiotherapy and pelvic-floor rehabilitation
- Outreach pathways (hospitals/NGOs/peripheral clinics) to keep care accessible.
The result is a pathway that safeguards nerve function and optimizes long-term outcomes.
So—can L4 and L5 cause bladder problems? Yes. When a disc at L4–L5 compresses nerve roots (or the cauda equina), bladder signaling can falter—sometimes subtly (urgency, hesitancy), sometimes dramatically (retention/incontinence). The good news: with early recognition, appropriate imaging, and a tailored plan—from conservative therapy to minimally invasive decompression—most people can protect or regain bladder function and return to normal life.
If you’re experiencing back/leg symptoms plus any change in urination, don’t wait. Get a spine evaluation promptly.
Book Your Consultation Today
Our Synapse Spine Clinic is located in Vasai, Bandra, Andheri, Mira Road, Vile Parle, Chembur, Borivali, and Virar.
📞 Contact Numbers with call button for each number:
+91 81698 45056 | +91 93726 71858 | +91 93211 24611 | +91 74998 98303